PRESS RELEASE
Tallaght University Hospital (Dublin, Ireland) and Aseptika Ltd (Cambridgeshire, UK) develop a new digital solution to support respiratory patients manage their condition
13th October 2021: Cambridgeshire, UK
The pandemic has created many problems but it has also driven innovation and invention as clinical innovators find new ways to help their patients.
Doctors and Physiotherapists at Tallaght University Hospital (TUH) in Dublin wanted to develop a simple app to enable patients with chronic obstructive pulmonary disease (COPD) to exercise at home. One of the treatment strategies that has clearly demonstrated efficacy in reducing exacerbations and therefore hospitalisations, enhancing patients’ quality of life and enabling self-management is Pulmonary Rehabilitation (PR). These classes incorporating exercise and education run for eight weeks and are given to small groups of patients by a Physiotherapist at the Hospital.
The onset of the COVID-19 pandemic forced suspension of face-to-face PR classes and TUH physiotherapists had to find alternative ways to enrol patients in Pulmonary Rehabilitation at home.
The TUH clinical team proposed the development of an app/technology to deliver short video clips of these exercise classes that patients could participate in at home and to motivate patients to have a brisk daily walk.
The challenge was how to make these suitable for patients with different levels of physical fitness and how to increase the exercise goals automatically for patients but adapted to each patient’s individual abilities.
Dr John Cullen, Consultant in General Internal & Respiratory Medicine in the Acute Medical Unit at TUH, as well as Clinical Senior Lecturer in Respiratory Medicine in Trinity College Dublin, was part of the TUH clinical team that posed this challenge to small companies via a process called Small Business Innovation research (SBIR), a collaboration between TUH, HSE and Enterprise Ireland. He said,
“None of the currently available apps and technologies addressed our specific needs, that is how to (1) incrementally and automatically increase activity levels based on patient progress; (2) tailor the exercise programme according to the patient’s ability to exercise; and (3) incentivise this activity to ensure ongoing and long-term patient engagement with the exercise programme. Most of the currently available apps are so-called “flat apps” with no in-built mechanism for automation or progressing. We needed something innovative and unique, and this is the challenge we presented to the companies.”
Working with the Health Services Executive, the Hospital used a pre-procurement initiative to fund the development of a prototype from two companies, one of which was UK-based Aseptika, a medical device company specialising in remote patient monitoring and a keen interest in motivating physical activity.
Kevin Auton, Managing Director of Aseptika commented,
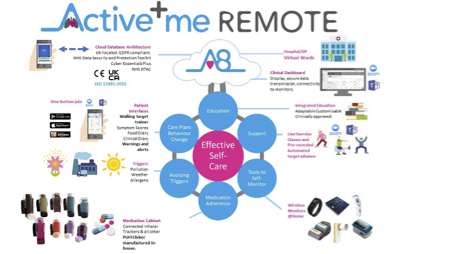
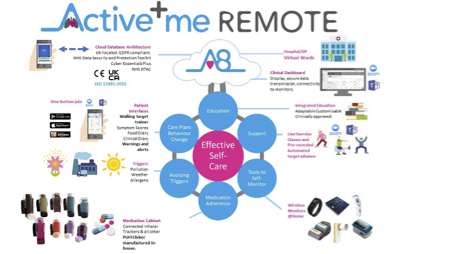
“What attracted us to this opportunity was the very detailed description of the problem the clinical team needed to solve. What they wanted was very close to our existing product, but their vision would push this to an entirely new level of automation for health service delivery. This new product was prototyped at record speed in just four months.
It works by asking each patient how breathless their prescribed exercise class or walking is making them.
As patients get fitter over time, knowing how much exercise they are doing and how they are coping with their activity goals, it automatically adjusts the exercise programme up or down for each patient.
How they are doing is feedback to the clinical team, along with information about how well they are feeling, whether they have had another flare-up of their lung condition, what medication they are taking and whether they feel well enough to continue to exercise.”
In the next stage of the development programme, the new app called Active+me REMOTE Recovery, will be developed further and will be tested by patients at TUH along the way to ensure they are involved directly in its design before it is tested formally at the Hospital.
The Hospital team aim to be able to roll-out this new product as a medically-approved app in the EU and UK during 2022.
If these trials are successful, the clinical team hope to see the app made available to all patients in Ireland that have COPD to help them self-manage at home. It will also help hospitals recover from the high demands placed on them by the pandemic.
–Ends–
Notes to the Editor
Background information - Chronic Obstructive Pulmonary Disease in Ireland
Chronic obstructive pulmonary disease (COPD) is a disease of the lungs characterised by airflow obstruction. This airflow obstruction is usually progressive and only partially reversible. The disease is associated with increasing dyspnoea (breathlessness) and in more severe cases can be associated with exacerbations of the disease, which may require intervention either in primary care, attendance at the hospital or even admission to hospital. It is a significant cause of mortality in Ireland and compared with other European countries, Ireland has one of the highest age standardised death rates from COPD.
In 2016 Ireland was noted as having the highest hospitalisation rates per 100,000 head of population in the OECD in relation to COPD. It is estimated that 380,000 people are living with COPD yet only 110,000 are diagnosed. It is particularly prevalent in the more vulnerable in society including people from areas with high social deprivation.
Tobacco smoking is the most important risk factor for the development of COPD. Tobacco smokers have a higher prevalence of respiratory symptoms, lung function abnormalities and mortality from COPD than non-smokers. However, in most studies up to 15% of patients with COPD are non-smokers. Many patients with COPD have been ex-smokers for many years. A view of COPD as a smoker’s disease is not accurate and can act to prevent COPD patients from getting appropriate resourced care (Health Services Executive website, 12.08.2021).
Note
This work was commissioned and funded by the SBIR Ireland programme. The views expressed in the publication are those of the author(s) and not necessarily those of the SBIR Ireland programme or its stakeholders.
Further information
Activ8rlives, Activ8rlives.com, Asthma+me, Active+me REMOTE Recovery and BuddyWOTCH are trademarks of Aseptika Ltd.
For further details, please contact Jessica Auton on +44 (0)1480 352 821 or email jessica.auton@aseptika.com
Aseptika Ltd www.activ8rlives.com
Aseptika Ltd began developing Activ8rlives in 2010 and is currently developing its fourth generation of integrated systems, which can be used by consumers and their healthcare service providers using a wide range of platforms or devices to better enable effective and easy self-monitoring.
Incorporating sensors and monitors ranging from consumer accessories to in vitro diagnostics (IVDs). Our focus is: respiratory and cardiovascular disease, cancer, promoting physical activity and weight management. Aseptika Limited has been certified by BSI to ISO 13485:2016 under certificate number MD691414.
Tallaght University Hospital
TUH is one of Ireland’s largest acute teaching hospitals, with adult, psychiatric and age-related healthcare on one site. The Hospital has 495 adult beds with over 3,000 people on staff. The Hospital is a provider of local, regional and national specialties. It is also a national urology centre, the second largest provider of dialysis services in the country, a regional orthopaedic trauma centre and a designated trauma unit. The Hospital also has 67 paediatric beds under the governance of Children’s Health Ireland and 52 mental health beds under HSE governance.
TUH is one of the two main academic teaching hospitals of Trinity College Dublin - specialising in the training and professional development of staff in areas such as medicine nursing, health and social care professionals, emergency medicine and surgery, amongst many others. TUH is part of the Dublin Midlands Hospital Group which serves a population of over 1.2 million across seven counties.
(V1.0) Final
